Calciphylaxis – Diagnosis and Management

As we have seen in previous weeks, calciphylaxis is a severe and complex syndrome involving vascular calcification, thrombosis, and skin necrosis. Calciphylaxis occurs almost exclusively in patients with advanced chronic kidney disease (CKD), and has a dismal mortality rate of around 80 percent (with a 1-year mortality greater than 50 percent).(1)
No Evidence-Based Medical Treatments
With such a discouraging prognosis, it is clear that treatment options for calciphylaxis still have some way to go. In fact, there are no evidence-based medical treatments available, with medical strategies currently based purely on case reports or personal experience.(2) As with many poorly-understood conditions, the key to the management of calciphylaxis therefore lies in strategies to prevent the condition from developing in the first place. This involves interventions such as controlling blood sugar levels in a diabetic patient(2) and normalizing metabolic parameters as far as possible using dialysis techniques and medications.(3)
Diagnosis of Calciphylaxis
If calciphylaxis is suspected, the diagnosis should be confirmed histologically in order to differentiate the condition from other similar vasculopathies which may be presented by the same patient types.(3) Once diagnosis has been confirmed, effective wound care becomes the cornerstone of management, and should be based around periodic debridement of necrotic tissue and proven wound management strategies.(1)
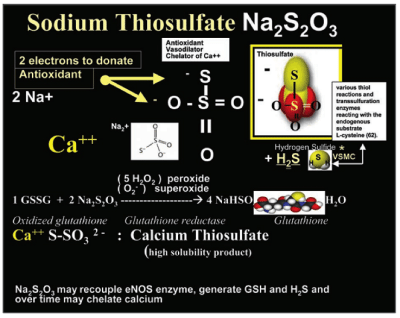
Parathyroidectomy in the treatment of calciphylaxis has been reported to benefit some patients with primary hyperparathyroidism, but its use remains controversial.(1) Other potential medical options include use of the bisphosphonates, sodium thiosulfate therapy and the calcimimetic, cinacalcet, although no randomized evidence supports the use of any of these approaches.(1) One proposed mechanism of action of sodium thiosulfate therapy in calciphylaxis is shown below.
Systemic corticosteroids should be avoided in calciphylaxis as they may exacerbate arteriolar calcification.(1) Hyperbaric oxygen therapy has been reported to be beneficial in the treatment of cutaneous ulcers, although again the evidence is anecdotal.(1) Pain relief should be offered through opioid-based preparations, as byproducts of morphine can cause hypotension, reducing blood flow in the arterioles and increasing risk of thrombosis.(1) Systemic antibiotics may used when indicated.(1)
The lack of evidence for the benefit of any treatment for calciphylaxis is disappointing, and contributes to the overall dismal prognosis for this condition. It is, therefore, the responsibility of the individual healthcare professional to implement management strategies based on previous experience and that of professional colleagues. The case-report evidence which is available may be studied as part of an ongoing professional development program, such as wound care certification.
Learn More With Our Wound Care Education Options
Interested in learning more about wound care and certification? Browse through our wound care certification courses for information on our comprehensive range of education options to suit healthcare professionals across the full spectrum of qualifications and experience.
References
- Bhambri S, Bhambri A, Del Rosso JA. Calciphylaxis: A review. J Clin Aesthet Dermatol 2008; 1: 38-41
- Brandenburg VM, Cozzolino M, Ketteler M. Calciphylaxis: a still unmet challenge. J Nephrol. 2011;24(2):142-8.
- Sowers KM, Hayden MR. Calcific uremic arteriolopathy: pathophysiology, reactive oxygen species and therapeutic approaches. Oxid Med Cell Longev. 2010;3(2):109-21.
Potential mechanisms of sodium thiosulfate in calciphylaxis, allowing for its antioxidant, vasodilator and chelation properties3
Reproduced from Sowers KM, Hayden MR. Calcific uremic arteriolopathy: pathophysiology, reactive oxygen species and therapeutic approaches. Oxid Med Cell Longev. 2010;3(2):109-21.

This is a venous ulcer. It is located in the gaiter area,is irregular shaped, shallow with slough tissue large. It looks like it is swollen. Would remove slough maintain moisture control bioburden and use compression.