Pathogenesis of Calciphylaxis

Calciphylaxis, a rare condition involving subcutaneous vascular calcification and cutaneous necrosis, is most commonly seen in patients with renal failure where it has a dismal mortality rate of up to 80 percent.(1)
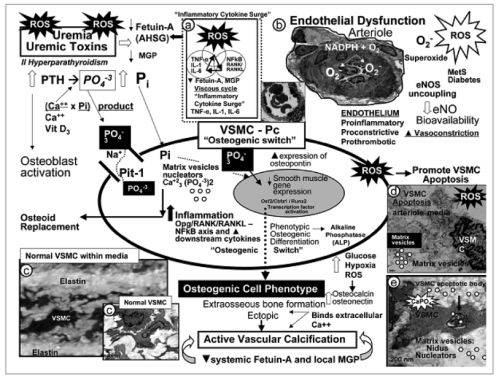
Calciphylaxis is a complex disorder associated with multiple histologic abnormalities and a multifactorial etiology.(1-3) The exact pathogenesis of the condition is unclear, and a full discussion is beyond the scope of this article. However, it is thought that in the initial stages of the disease, the presence of uremia and the decrease of local vascular calcification inhibitory proteins causes the vascular smooth muscle cells (VSMCs) to differentiate into osteoblast-like cellular phenotypes. Bone morphogenic proteins induce de novo bone formation leading to calcification outside the bones. The nuclear factor kappa B (NFκB) and its receptor activator (RANK), levels of which are raised in chronic inflammatory states such as alcoholic steatohepatitis, chronic kidney disease, and end-stage renal disease, also play an important role in bone homeostasis and vascular calcification. In addition, cytokines such as tumor necrosis factor alpha (TNFα), interleukin-1 (IL-1) and interleukin-6 (IL-6), which are elevated in obesity, contribute to the pathogenesis. The elevated concentration of reactive oxygen species (ROS) in uremia is also thought to be important in the development of calciphylaxis, leading to an inflammatory cytokine surge, VSMC apoptosis, endothelial dysfunction, and a decrease in bioavailable nitric oxide (NO). The complex interactions of some of these underlying systems are shown in the figure below.
Molecular Research
Because of the large number of interacting systems involved in the pathogenesis of calciphylaxis, considerable research effort is currently devoted to understanding the exact nature of the different processes involved. It is hoped that a fuller understanding of the condition on a molecular level will provide new treatment options for this devastating disease, and improve the currently pitiful prognosis for this condition.
If you are interested in learning more about the pathogenesis of calciphylaxis, you may decide to study for a further professional qualification in wound management.
Learn More With Our Wound Care Education Options
Interested in learning more about wound care and certification? Browse through our wound care certification courses for information on our comprehensive range of education options to suit healthcare professionals across the full spectrum of qualifications and experience.
Figure: Potential mechanisms involved in the pathogenesis of calciphylaxis.(2)
Reproduced from Ref. 2
References
- Bhambri S, Bhambri A, Del Rosso JA. Calciphylaxis: A review. J Clin Aesthet Dermatol 2008; 1: 38-41
- Sowers KM, Hayden MR. Calcific uremic arteriolopathy: pathophysiology, reactive oxygen species and therapeutic approaches. Oxid Med Cell Longev. 2010;3(2):109-21.
3. Brandenburg VM, Cozzolino M, Ketteler M. Calciphylaxis: a still unmet challenge. J Nephrol. 2011;24(2):142-8.

very interesting article…thanks
My name is, Lisa. I was diagnosed with Calciphylaxis in April of 2015. After 9-months of, Sodium Thiosulfate treatment (infusion therapy 3x/week) I’m entirely healed…with no sign of ulcers, but I imagine the scars will be forever. My Calciphylaxis diagnosis was originally considered “idiopathic”, but was eventually attributed to alcoholic liver disease. Since diagnosis I’ve been 100% sober and eating a “paleo” diet. All things considered, I’m extraordinarily blessed…to have my life, legs and health. As of now, the only evidence of the disease is in photos!