Diabetic Foot Ulcer Classification Systems
It is crucial to apply a standardized measurement system to evaluate whether a diabetic foot ulcer is responding to care, as a result several classification systems have been proposed.
At the present time no specific system has been universally accepted. Even so, most clinicians use one of the available systems when assessing and documenting a diabetic ulcer.
In this article we will discuss two commonly used classification systems; The Wagner diabetic foot ulcer grade classification system and the University of Texas diabetic foot ulcer classification system.
The Wagner Diabetic Foot Ulcer Grade Classification System
The Wagner diabetic foot ulcer classification system assesses ulcer depth and the presence of osteomyelitis or gangrene by using the following grades:
- Grade 0 – intact Skin
- Grade 1 – superficial ulcer of skin or subcutaneous tissue
- Grade 2 – ulcers extend into tendon, bone, or capsule
- Grade 3 – deep ulcer with osteomyelitis, or abscess
- Grade 4 – partial foot gangrene
- Grade 5 – whole foot gangrene
Note: While the wound shown in the above image may appear to be a grade 3 ulcer, upon assessment no abscess or osteomyelitis was found. Beneath the superficial necrotic tissue was exposed tendon.
The University of Texas Diabetic Foot Ulcer Classification System
The University of Texas system grades diabetic foot ulcers by depth and then stages them by the presence or absence of infection and ischemia:
- Grade 0 – pre-or postulcerative site that has healed
- Grade 1 – superficial wound not involving tendon, capsule, or bone
- Grade 2 – wound penetrating to tendon or capsule
- Grade 3 – wound penetrating bone or joint
Within each wound grade there are four stages:
- Stage A – clean wounds
- Stage B – non-ischemic infected wounds
- Stage C – ischemic noninfected wounds
- Stage D – ischemic infected wounds
Additional Diabetic Foot Ulcer Classification Systems
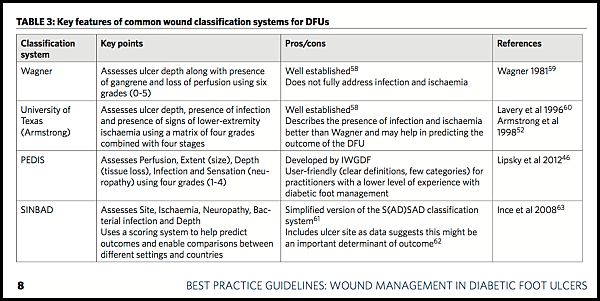
The following chart from Wounds International highlights additional classifications systems.
For detailed information on the above chart refer to “Best Practice Guidelines: Wound Management in Diabetic Foot ulcers”
Conclusion
While each system uses a different approach to classify a wound, similarly each system classifies the wound according to depth, presence of ischemia, and presence of infection.
Regardless of which classification system is used, it is essential that the system be used consistently across the healthcare team and be recorded appropriately in the patient’s records.
Want to Improve Your Wound Care knowledge?
If you’d like to improve your knowledge in advanced wound care and become wound care certified, we have a great course waiting for you. Our online wound care certification course is a perfect choice. Whether you’re just starting out or you’ve been working with wounds for years, you’ll find this course helpful. You’ll learn what evidence based wound management is and how you can achieve wound care certification. The course will help you gain a solid wound care foundation that will benefit your patients, your employer and your career.



Thank you for the information on Diabetic foot ulcer classification systems. I had no idea that diabetic foot ulcers could get so bad they reach tendons or even the bone. I wonder how you catch an ulcer early, or how to treat one that’s gone so deep it affects a tendon or bone.
I good number of case recorded for diabetic foot
Where tight glycaemic controlled is very very importent
So true!! Tight glycemic control is essential to diabetic wound healing. Thanks for your input.
A diabetic has a heel ulcer completely covered by eschar. Should this be “Staged” or “Graded” according to the Wagner Grading Scale. If “Graded”, what would be the Grade ?
I should mention that it developed as a result of pressure.
Hi Matthew, That is a difficult question one that many professionals struggle will. The cause of the ulcer is clearly related to both disease processes and both pressure and diabetes will need to be addressed. For documentation purposes, the PRIMARY cause of the ulcer would be documented. If the ulcer was caused by pressure and is completely covered by eschar, it would be documented as an unstageable pressure ulcer with the comorbidity of diabetes. For more infomation refer to the following article: http://www.diabeticfootcanadajournal.ca/download/content/4588
Thank you for that. Once the eschar is removed and is visualuzed, would the classification ever be converted to a Wagner Grade or does it remain “Staged” ?
If the primary cause of the wound was pressure it would remain a pressure ulcer.
Thank you so much. This topic at our wound center seems to raise more questions the more we talk about it. If we derermine that a diabetic foot ulcer should be graded and is completely covered by eschar, what Wagner Grade would it be ? Thanks
The wound would need to be debrided in order to accurately stage. Following is a great article on staging: https://www.woundsresearch.com/article/8706
Can a Wagner classification be given to an infected below knee amputation residual limb or does it have to be a foot?
Kathy,
Wagner classifications are given to diabetic foot ulcers and lesions, not limbs. Hope this helps!
Can a Wagner grade 1 Ulcer also be considered a full thickness wound?
Hi Alex! Thanks for your inquiry. A Wagner grade 1 is considered a superficial ulcer, not a full thickness wound.
Thank you for the answer! I do have a followup question. If you have a diabetic wound that extends into the subcutaneous layers, lets say 2cm, but does not reach tendon, bone, or joint would that be considered a Wagner grade 1 or grade 2?
Alex,
You can use this resource for more information and illustrations http://nhafp.org/pdf/intro-to-wound-care.pdf
Is anybody aware of any licensing for the Wagner Diabetic Foot Ulcer Grade Classification System?
Thank you.. I found this information very valuable. Thank you
Are non-pressure ulcers “reverse-graded” as they heal – or are they reported at their deepest like pressure ulcers?
i am doing research on diabetic foot ulcers dressings.I want to compare between papya dressing and povidone 10 % dressing.i need a criteria to declare diabetioc foot ulcer is healed .which is practical and can be documented .
regards
Dr amir rasool
[email protected]
Hey Dr. Amir- our best recommendation would be to get the assistance of a wound certified professional in your area. You can find one through the ABWM’s website directory. Best of luck!
Can a Wagner DFU ever be “back-staged ” e.g. from a Grade 2 to a grade 1 or stage C to stage A – once improved?
Hey Heidi, the short answer is No. Only pressure injuries are back staged. Thanks for your interest in wound care!
As a diabetic ulcer heals, will the Grade for that wound improve? Or is it like a pressure ulcer and the stage never changes after it is staged?