Hyperbaric Oxygen Therapy
Wound ischemia is thought to be the most common cause of healing failure in a chronic wound.1 Furthermore, the rate of wound healing can be correlated directly with the level of tissue oxygenation. There is, therefore, a strong rationale for the use of oxygen therapy to promote wound healing in difficult-to-heal wounds.1
Hyperbaric oxygen therapy (HBOT) refers to an adjunctive treatment modality in which a patient inhales 100% oxygen under an elevated pressure for a pre-specified period of time.1–4 Pressure is applied at 2 to 3 atmospheres absolute, which is the sum of the atmospheric pressure (1 atm) plus an additional hydrostatic pressure equivalent to one or two atmospheres.2 Treatment may be performed individually or in a hyperbaric oxygen chamber capable of treating up to 14 patients simultaneously. Treatments tend to last around 1.5 to 2 hours, depending on the indication, and may be repeated between one and three times a day.2
Oxygen therapy in various forms has been used for various ailments including leprosy since the mid seventeenth century. However, it was not until the 1970s when this modality was researched systematically in a series of well-executed randomized trials.1
Rationale and Mechanism of Action
Oxygen is essential to normal wound healing, playing a pivotal role in almost all of the processes involved. The condition in which tissue oxygen levels are reduced to below around 30 mmHg is known as ischemia or tissue hypoxia, and this state fundamentally impairs the normal cellular processes and inhibits wound healing.1
The roles of oxygen in the wound healing process are too numerous to cover in depth. However, as examples, oxygen is essential in all cellular metabolic processes, including fibroblast proliferation, collagen synthesis, exportation of collagen from the fibroblast cell membrane and neoepithelialization.1 Moreover, angiogenesis at the edges of a wound is driven by the oxygen gradient between the poorly oxygenated wound center and oxygen rich wound periphery. Improved oxygen delivery enhances this oxygen gradient and promotes wound repair. Finally, a lack of oxygen reduces the resistance of tissues to infection, while high oxygen concentration enhances the ability of leukocytes to produce free radicals, causing bacterial death.1
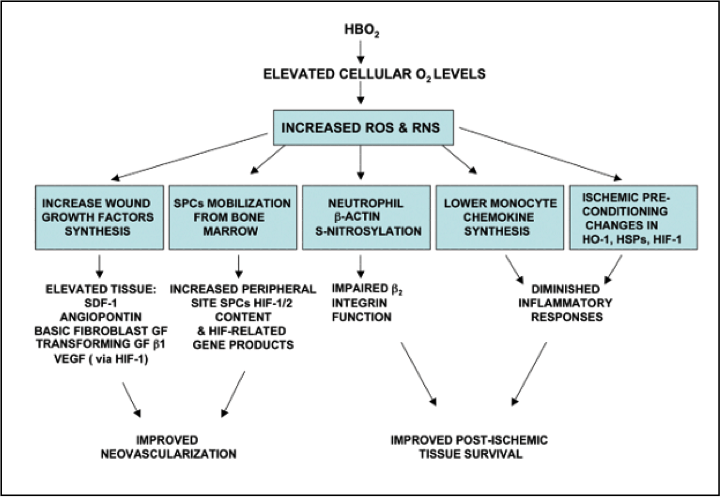
HBOT promotes wound healing by restoring or increasing oxygen levels to allow the normal wound repair processes to occur. The principal mechanisms of this modality are based the on intracellular generation of reactive species of oxygen and nitrogen, which are known to play a central role in cell signal transduction cascades (see Figure 1).
Uses of and Evidence for Hyperbaric Oxygen Therapy
The benefit of HBOT has been shown in the treatment of hypoxic and ischemic wounds in randomized trials and systematic reviews.1,3 For example, the modality has been shown to be effective for patients with diabetic foot ulcers, and to significantly reduce the risk of major amputation and improve the chance of healing at 1 year.1.3 One literature review based on a combination of clinical trials, nonrandomized trials, cohort studies, retrospective analyses, and case series showed evidence that HBOT promotes healing of arterial ulcers, calciphylactic ulcers, refractory vasculitic ulcers, and osteomyelitis, as well as the success of treatment for compromised flaps and grafts. Two Cochrane systematic reviews, however, showed that the potential value of HBOT for open fractures and burns was unclear.1
The most recent systematic review identified five separate randomized trials that evaluated the effectiveness of hyperbaric oxygen therapy compared to other interventions on wound healing.3 One trial in 36 patients showed that significantly more crush wounds healed with HBOT than with sham HBOT [relative risk (RR) 1.70, 95% confidence interval (CI) 1.11–2.61]. This study also reported that significantly fewer additional surgical procedures were required with HBOT (RR 1.60, 95% CI 1.03–2.50), and significantly less tissue necrosis was found (RR 1.70, 95% CI 1.11–2.61). A further study evaluated showed that the rate of burn-wound healing was significantly greater with HBOT compared with routine burn care (P < 0.005). A British trial showed that HBOT resulted in a significantly higher percentage of healthy graft area in split skin grafts (RR 3.50, 95% CI 1.35–9.11), while a Chinese trial showed that HBOT did not significantly improve flap survival in patients with limb skin defects. On the basis of a systematic review of these trials, the authors concluded that HBOT appears effective for the management of acute, difficult-to-heal wounds.3
Risks and Side Effects
HBOT is generally well tolerated, and is not normally considered to pose significant risks to patients. The most frequent side effect is middle ear barotraumas, which can present as hyperemia of the ear drum to ear drum perforation in the most serious case. Other serious, but rare, side effects include brain oxygen toxicity, oxygen lung toxicity, and transient myopia.1
There are a small number of absolute contraindications to HBOT, of which the most important is uncontrolled pneuomothorax. Other absolute contraindications include recent or current treatment with adriamycin, bleomycin, doxorubicin, or disulfiram. The modality should also be used with a degree of caution in individuals with respiratory infection, severe asthma or chronic obstructive pulmonary disease, fever, steroid treatment, seizure disorders, history or optic neuritis, and claustrophobia.1
Conclusion
There is good, randomized evidence available for the effectiveness of HBOT as adjuvant treatment for hypoxic wounds, and this modality is recommended by different medical societies, health organizations and healthcare agencies.1 However, it should be remembered that HBOT is only ever an adjuvant approach to mainstream wound management. The management of all chronic wounds should be built around the fundamentals of a multidisciplinary approach and optimal topical wound treatment.1
Learn More With Our Wound Care Education Options
Interested in learning more about wound care and certification? Browse through our wound care certification courses for information on our comprehensive range of education options to suit healthcare professionals across the full spectrum of qualifications and experience.
References
- Kulikovsky M, Gil T, Mettanes I, Karmeli R, Har-Shai Y. Hyperbaric oxygen therapy for non-healing wounds. Isr Med Assoc J. 2009 Aug;11(8):480-5. Review.
- Thom SR. Hyperbaric oxygen: its mechanisms and efficacy. Plast Reconstr Surg. 2011 Jan;127 Suppl 1:131S-141S.
- Eskes AM, Ubbink DT, Lubbers MJ, Lucas C, Vermeulen H. Hyperbaric oxygen therapy: solution for difficult to heal acute wounds? Systematic review. World J Surg. 2011 Mar;35(3):535-42.
- Sen CK. Wound healing essentials: let there be oxygen. Wound Repair Regen. 2009 Jan-Feb;17(1):1-18.

It stood out to me when you explained that hyperbaric oxygen therapy promotes wound healing. Can hyperbaric oxygen therapy be used to help a broken bone heal more quickly? As far as I know, broken bones tend to take a long time to heal, so using innovative treatment methods to speed up the process makes a lot of sense.