Modalities Utilized in Wound Healing: Negative Pressure Wound Therapy (NPWT)
Negative pressure wound therapy, also known as NPWT, is a relatively new modality in wound healing; however, there is much evidence, both scientific and anecdotal, to support its use. Let’s take a look at how negative pressure wound therapy works and why it is increasingly being used for wounds that have failed to heal using other, more traditional, modalities.
Functions
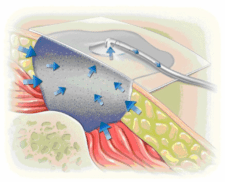
Negative pressure wound therapy (NPWT) utilizes a pump that applies a prescribed amount of negative pressure to the wound bed. Negative pressure is thought to promote wound healing by:
- Increasing capillary filling
- Improving lymphatic flow
- Increasing local blood flow
- Enhancing oxygenation through improved tissue perfusion
- Encouraging cellular proliferation, angiogenesis and release of growth factors
- Improving control of wound exudate
- Increasing granular tissue formation
- Decreasing wound and periwound edema
- Enhancing epithelialization
- (Possibly) decreasing bioburden
Indications/Precautions
NPWT has been used to treat almost every wound type, including pressure ulcers, diabetic ulcers, vascular and arterial ulcers, traumatic wounds, chronic/nonhealing wounds, wounds with exposed bone, tendon and/or other subcutaneous tissues, burns and skin grafts/muscle flaps. Studies have shown a favorable response of all of these wound types to NPWT.
However, there are a few exceptions. NPWT is contraindicated when the wound is dry or necrotic, there is a malignancy underlying the wound, the patient has untreated osteomyelitis, there are exposed blood vessels present and when there is active bleeding or the patient is on an anticoagulant. Negative pressure may cause increased bleeding; if NPWT is used on a wound that is bleeding or on a patient taking anticoagulant therapy, caution should be used. In these cases, the amount of negative pressure applied should be reduced.
How to Perform
As with other modalities, the wound bed should be prepared prior to the application of NPWT. This may mean that the wound is debrided to rid the wound of any necrotic or nonviable tissue. Once the wound bed is ready, you should cut the foam to match the size of the wound. There are two types of foam available: black (polyurethane) foam and white (polyvinyl alcohol) foam. Black foam should be used to promote the formation of granulation tissue and wound contraction; white foam should be used if the black foam is very uncomfortable for the patient (due to its increased density) or when you want to encourage wound epithelialization. You should moisten the foam prior to application as the foam is hydrophilic. Areas of tunneling or undermining can be lightly packed with foam. Important to remember is that when multiple pieces of foam are used, they must be in contact with each other in order to maintain equal dispersal of pressure/suction. The collection canister is attached to the pump, and the free end of the tubing is attached to the dressing through a small hole that is created in the dressing, so that the tubing is lying within the wound bed. The tubing can create pressure on the periwound, therefore you should consider using a dressing to prevent this pressure being applied (such as a hydrogel or hydrocolloid).
Next, cover the wound and intact periwound area with a film drape. Open the tube clamps and turn the pump on at the prescribed pressure to allow wound fluid and bacteria to travel to the collection canister, which can typically hold anywhere between 300 and 1000 millilitres (mL). Pump pressure can be adjusted between 50 and 175 mmHg. Higher pressures up to 125mmHg have been shown to result in a maximal increase in blood flow. When increasing the pressure, adjust slowly so as not to cause pain. The pump may be set to intermittent or continuous (some studies have shown superior results achieved using intermittent suction. The dressing can remain in place for up to 72 hours. Change the dressing more frequently if the wound is infected (change every 12 to 24 hours).
Patient Considerations
Some patients find that they experience pain during treatment and/or when the dressing is changed. Pain can be decreased by using the white foam or by using lower suction pressures. Adding saline to the foam prior to dressing removal can decrease pain associated with dressing changes. Pain medications can also be administered one half hour prior to dressing changes if necessary to reduce pain, or regularly to decrease pain that occurs during therapy if the above suggestions are ineffective.
Advantages/Disadvantages of NPWT
The biggest disadvantage of NPWT is cost. It has been estimated that each dressing costs approximately $100.00. On the other hand, if the wound heals faster money can be saved over time. Advantages include superior exudate control and maintenance of a warm, moist wound environment.
NPWT is gaining in popularity for the treatment of chronic wounds. If you enjoyed learning about negative pressure wound therapy, perhaps you might enjoy the learning resources available at WoundEducators.com. If you are interested in wound care, consider becoming certified in wound management. Wound Educators is the foremost online wound education forum, offering wound certification courses for healthcare professionals.
Sources:
Meyers, B (2008). Wound Management: Principles and Practice. 2nd edition. Pearson Prentice Hall. Upper Saddle River, New Jersey. pg. 177-179.
Negative pressure wound therapy. World Wide Wounds. Updated December 2010. http://www.worldwidewounds.com/2010/December/Oien/NPWT.html