Modalities Utilized in Wound Healing: Electrical Stimulation
Electrical stimulation is a relatively new phenomenon in wound care. While some studies have shown little to no improvement with the use of electrical stimulation, many other studies have found that wound healing may be greatly enhanced with the use of this modality.
Functions
How does electrical stimulation aid in wound healing? The following are the ways in which electrical stimulation is thought to aid in wound healing:
- facilitates debridement- electrical stimulation is thought to facilitate the process of autolytic debridement
- stimulates galvanotaxis- galvanotaxis is the stimulation of cells along an electrical gradient. Electrical stimulation may attract keratinocytes, macrophages, neutrophils, fibroblasts and endothelial cells to the area of injury. Applying electrical stimulation can thus be said to enhance all of the phases of wound healing by enhancing the migration of cells necessary for regeneration and repair of the affected area
- decreases edema-it is thought that electrical stimulation reduces edema within the area treated, perhaps by decreasing permeability of the microvasculature which is induced by inflammation and injury
- restores the current of injury-when there is a break in the skin, the skin’s electrical resistance is disrupted, which makes the wound electropositive in comparison to the surrounding tissues. This change in polarity triggers the wound healing cascade. In chronic wounds, this current of injury is thought to be arrested. Applying electrical stimulation may mimic the flow of current which normally occurs, stimulating wound healing. Drying of the wound bed also impedes the current of injury, which can slow wound healing. This further supports the current thinking behind moist wound healing.
- increases the ability to fight off bacteria-electrical stimulation may have an antibacterial effect because macrophages and neutrophils are attracted to the anode and the cathode (positive and negative electrode), although this effect seems to be greater at the cathode.
- stimulates blood flow- applying electrical stimulation enhances blood flow to the wound being treated, resulting in an increase in tissue partial pressure of oxygen and higher capillary oxygen tension. Increase blood flow stimulates wound healing, and greater oxygen availability increases the ability to fight off infection, as well as improving the body’s ability to build new tissue.
- cell proliferation-electrical stimulation results in a general increase in fibroblasts, platelets, macrophages and endothelial cells. It also enhances collagen synthesis, granulation tissue formation and DNA synthesis, which speeds up the repair process and improves tensile strength.
Indications/Precautions
Electrical stimulation should be reserved for chronic wounds or for patients who are at a high risk for delayed wound healing. Electrical stimulation should not be used when osteomyelitis is present because electrical stimulation cannot heal a bone infection. Stimulating wound healing would thus facilitate wound closure in these types of wounds, which would only result in formation of an abscess. Electrical stimulation should not be used when topical agents containing heavy metal ions are present. It should also not be used on actively bleeding wounds before hemostasis is achieved. Caution should be used in patients with decreased sensation, such as diabetic patients with neuropathy.
How to Perform
There are three techniques which may be used to apply electrical stimulation to stimulate wound healing:
- Direct technique-in this technique, electrical stimulation is applied directly to the wound bed. Prior to applying electrical stimulation, the wound is debrided and irrigated as necessary. Gauze moistened with saline is placed within or on the wound bed and is covered with a carbon electrode. You may choose to apply a moisture barrier or a skin sealant to protect the periwound and prevent maceration in areas where the moist gauze is in contact with intact skin. The electrodes are then secured in place. The return electrode is prepared in a similar fashion and is placed anywhere that is convenient, usually proximal to the wound. Following treatment, you should perform any measurements prior to dressing the wound. If carbon electrodes are used they should be cleansed with an approved disinfectant according to infection control guidelines.
- Immersion technique- in this technique, the area with the wound is immersed in a nonmetal basin filled with water. The treatment electrode is placed in the basin with the contact side down. This technique may be used for patients with foot or hand ulcers. Hyperhydration and dependent positioning are two factors which must be considered when using this technique.
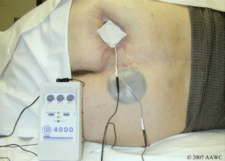
- Periwound technique-this technique involves the application of electrodes to an intact periwound, rather than to the wound bed itself. The treatment electrodes are positioned so as to straddle the wound bed. The advantage of this technique is that wound dressings may be kept in place, decreasing the potential for wound contamination.
Stimulation frequency should be between 80 and 125 Hz. If the pulse interval can be adjusted it should be set at between 50 and 100 µs (microseconds). The intensity of stimulation should be somewhere between 75 and 200 volts and should produce a comfortable paresthesia for the patient. When the patient has decreased sensation, the intensity should not exceed 200 volts. Treatments should be between 45 and 60 minutes in length, or 30 minutes if performed twice daily. Outpatient treatments are often scheduled for three times a week.
Patient Considerations
Patients may be apprehensive due to concerns regarding electricity, i.e. they may be afraid of being electrocuted. Careful explanation should be provided to the patient to prevent fear of the procedure. Monitor the patient for pain throughout the procedure, keeping in mind and electrical stimulation does not typically cause pain.
Advantages/Disadvantages
Advantages of electrical stimulation include the following:
- can be used in any setting
- less time is required for setup and cleanup than whirlpool treatments
- does not typically cause pain or discomfort
Electrical stimulation may be more time-consuming than whirlpool treatments or pulsed lavage. There is also a risk of cross-contamination if equipment is not cleaned properly. In addition, electrical stimulation cannot be used on wounds that are very large.
In the next section, we will discuss the use of negative pressure wound therapy (NPWT) in wound healing. If you enjoy learning about wound care, consider becoming certified in wound management. Wound Educators is the foremost online wound education forum, offering wound certification courses for healthcare professionals.
Sources:
Thakral, G., LaFontaine, J., Najafi, B., Kim, P. & Lavery, L. (2013). Electrical stimulation to accelerate wound healing. Diabetic Foot Ankle 2013. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3776323/
Meyers, B (2008). Wound Management: Principles and Practice. 2nd edition. Pearson Prentice Hall. Upper Saddle River, New Jersey. pg. 169-173.

Just to let you be aware, electrical stimulation is not a new treatment. It is probably older than most of the new dressings in the last 10 years. I was doing electrical stimulation as a PTA 20 years ago.
Deidre
Where do you place the anode and cathode relative to the damaged nerve for regeneration? Thanks
It depends on which type of nerve injury ?
If neurotemesis (complete cut of nerve than use Galvanic stimulation and electrode placement should be proximal to injured site.
If neuropraxia ,or Axontemesis than faradic stimulation should be used and placement should be along the nerve pain and compression site because we want to glide ,stimulate and supply the nutrition to nerve for healing .
Direct application unique technology
Please more details