Prevent Scarring – Scarring Reduction
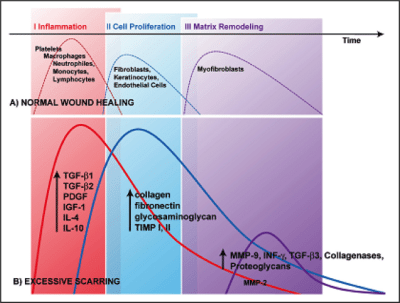
Excessive scar formation results from an abnormal physiologic response to an injury deep in the dermis, including burn injury, laceration, abrasion, or surgery (Figure 1).1–3 Elevated fibrous scars that extend beyond the borders of the original wound and usually occur after excision are known as keloids, while hypertrophic scars are maintained within the initial site of injury.
Why Prevention & Reduction of Scarring is Important
As well as having the potential to cause pruritus, pain, and contractures, by its very nature, excessive scarring is disfiguring and can adversely affect a patient’s self-confidence and quality of life. 1–3 It is therefore incumbent on the wound care practitioner to incorporate strategies for reduction of scarring into all wound healing protocols.
Strategies to Prevent Scarring
The best scar minimization strategies involve primary prevention, as promoted by following best evidence-based wound care protocols. However, in certain situations, scarring is inevitable and requires secondary management. A large number of studies have been conducted into hypertrophic scar and keloid formation, leading to a bewildering range of therapeutic strategies for the prevention or reduction of scarring. Typical approaches include the use of occlusive dressings and compression therapy, as well as corticosteroid injections, cryosurgery, excision, radiation therapy, and laser therapy, Pharmacological options include interferon (IFN) therapy, 5-fluorouracil (5-FU), doxorubicin, bleomycin, verapamil, retinoic acid, imiquimod 5% cream, tamoxifen, tacrolimus, botulinum toxin, and over-the-counter treatments.3
Ongoing Scar Research
Unfortunately, most available therapeutic approaches remain clinically unsatisfactory, due to an inadequate understanding of the complex mechanisms underlying the processes of scarring and wound contraction. Excessive scarring continues to be an area of intense research activity, and many investigational approaches are under development. Promising therapies reported to date include antiangiogenic factors, including phototherapy, as well as pharmacological approaches including vascular endothelial growth factor inhibitors (e.g., bevacizumab), transforming growth factor–beta3, tumor necrosis factor alpha inhibitors (e.g., etanercept), and recombinant human interleukin, which are directed at decreasing collagen synthesis.3
Improve Underlying Process Knowledge
Despite the large number of therapeutic approaches available to prevent excessive scarring, most options remain somewhat unsatisfactory, and scarring remains a significant burden for many patients. Major breakthroughs in this area can only be truly realized when our knowledge of the underlying processes involved in hypertrophic scar and keloid formation is improved.1
Figure 1. Differences between normal wound healing and excessive scar formation over time. In normal wounds, a balance is achieved between new tissue biosynthesis and degradation mediated by apoptosis and remodeling of ECM (A). During excessive scar formation, a dysfunction of the underlying regulatory mechanisms may lead to persistent inflammation, excessive collagen synthesis or deficient matrix degradation and remodeling (B). Reproduced from Gauglitz GG, Korting HC, Pavicic T et al. Mol Med 2011; 17(1-2): 113–125.1
Our Wound Care Education Options
Interested in learning more about wound care and certification? Browse through our wound care certification courses for information on our comprehensive range of education options to suit healthcare professionals across the full spectrum of qualifications and experience.
References
- Gauglitz GG, Korting HC, Pavicic T et al. Hypertrophic Scarring and Keloids: Pathomechanisms and Current and Emerging Treatment Strategies. Mol Med 2011; 17(1-2): 113–125.
- Juckett G, Hartman-Adams H. Management of Keloids and Hypertrophic Scars. Am Fam Physician. 2009; 80(3): 253–260.
- Berman B. Keloid and Hypertrophic Scar. Medscape 2012. Available at http://emedicine.medscape.com/article/1057599-overview