Wound Malignancies

Wound malignancy is a growing concern, particularly as the population ages and the ‘baby boomer’ generation reaches retirement. A malignant wound can result from tumor necrosis, fungating tumor cells, an ulcerating cancerous wound, or a malignant cutaneous wound;1 and rarely achieves satisfactory closure.2–3
Malignant wounds can have both ulcerative and fungating features and are often associated with odor and discharge, as well as pain, infection, and bleeding in some cases. However, diagnosis of wound malignancy tends to be problematic, as many affected wounds show no outward signs of cancer, such as a raised border or crusting. In particular epidermoid cancers may have many of the physical characteristics as chronic ulcers, meaning that these cancers often are overlooked especially in the elderly. A detailed medical history is, therefore, key to diagnosis of malignancy in any non-responding wound, and should include a thorough investigation into previous sun exposure and any personal or familial history of skin cancer.2 A biopsy or ellipse from all ulcers and wounds that do not respond to standard wound care protocols should also be obtained, as accurate diagnosis is pivotal to positive treatment outcomes.2
Example of fungating wound (Please note; the website you have selected is an external site hosted on a different server. We offer the link for your convenience. WoundEducators.com accepts no responsibility, and offers no expressed or implied warranty, for any external website.)
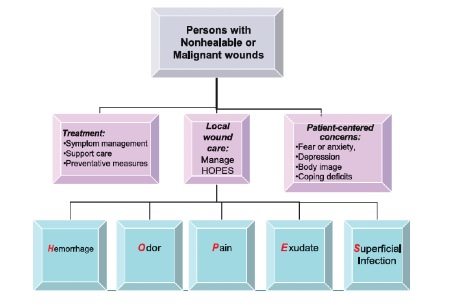
Management of malignant wounds tends to be palliative, but symptoms can usually successfully be controlled with good assessment and wound care practices. As with all wounds, the underlying cause should first be addressed where possible, while the psychological distress to the patient or caregivers should also be attended to as a matter of priority. Local wound care tends to be based on the HOPES strategy, in which issues relating to hemorrhage, odor, pain, and exudates are addressed (see Figure). Other supportive strategies to prevent exacerbation of existing wounds or the development of new lesions should also be implemented. In certain cases, topical application of anticancer agents may be considered to delay tumor progression.2
Learn More With Our Wound Care Education Options
Interested in learning more about wound care and certification? Browse through our wound care certification courses for information on our comprehensive range of education options to suit healthcare professionals across the full spectrum of qualifications and experience.
Figure. Wound management strategy for non-healable and malignant wounds.1 Reproduced from Woo KY. Sibbald RG. Local Wound Care for Malignant and Palliative Wounds. Adv Skin & Wound Care 2010; 23(9): 417–428
Editors Note: This post was originally published in December 2007 and has been revamped and updated for accuracy and comprehensiveness.
References
- Woo KY. Sibbald RG. Local Wound Care for Malignant and Palliative Wounds. Adv Skin & Wound Care 2010; 23( 9): 417–428
- Snyder RJ. Skin Cancers and Wounds in the Geriatric Population: A Review. Ostomy Wound Management. 2009; 64–76
- Payne WG, Naidu DK, Barko D. Wound healing in patients with cancer. Eplasty 2008; 8: e9.


I have taken your course that was offered on-line and also prep course and would like to obtain CEU’s. Do you offer this and where can I find.
So Interesting!!!