Moist Wound Healing
Moist wound healing is now the norm in wound care, rather than the dry gauze dressings of old. This is due to the fact that studies have shown that moisture actually speeds wound healing. The idea of moist wound healing was first defined during the 1960s. During this time, early pre-clinical and clinical research conducted by the British pioneer, George D Winter, first demonstrated the benefit of a moist environment in optimizing wound healing.
History of Moist Wound Healing Techniques
The concept of moist wound care really took off in the late ‘70s and ‘80s, and an explosion in the number of innovative dressing products, such as alginates, hydrogels, and foams, was seen throughout the 1980s and early ‘90s. For the first time, dressings were starting to be considered an important and active part of the healing process.
Our understanding has come a long way since the days of the first research of Dr Winter. We now understand why wound healing is promoted by a moist environment. This is due to several, parallel processes. Firstly, by preventing scab or crust formation over the wound bed, a moist wound environment eliminates the energy and time that would have been required for the body to breakdown these materials.
Secondly, keratinocyte-travel time and distance across the wound surface are also greatly reduced, as the cells are able to easily migrate across the moist wound bed rather than burrow underneath the wound bed to find a moist area upon which to move forward. A moist environment also traps enzymes within the wound bed, facilitating autolytic debridement. And finally, a moist wound environment preserves growth factors within the wound fluid, and increases fibroblast proliferation and collagen synthesis.
Advantages of Moist Wound Healing
Advantages of moist wound healing include the following:
- moist wounds heal 2-3 times faster than dry wounds
- a moist wound environment facilitates all three phases of wound healing; specifically, it decreases the intensity and length of the inflammatory phase, speeds the proliferative phase
- a moist wound environment decreases the amount of time it takes for the body to solubilize the crust that forms over dry wounds (scabs); by eliminating these barriers keratinocyte distance and travel time across the wound is reduced
- moist wounds facilitate autolytic debridement by trapping enzymes that are endogenously produced
- a moist wound environment preserves growth factors and other substances that promote cell growth and proliferation within the wound fluid
- moist wound healing increases the synthesis of collagen and the proliferation of fibroblasts
- moist wound healing hastens angiogenesis and wound contraction
- moist wound healing reduces wound pain in most patients
- moist wounds often have less scarring after healing takes place
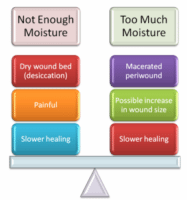
How Much Wound Moisture is Needed?
Unfortunately, there is no easy way to determine exactly how much moisture is needed for wound healing. However, there are some signs you can watch for that can help you determine when a wound is too dry or too wet- the trick is getting just the right amount of moisture without overdoing it. We’ve already discussed the advantages of moist wound healing, but what happens when wounds are too moist?
Wounds that are too wet can show delayed healing. The periwound can become macerated, which can lead to further skin breakdown. Macerated wounds more readily admit irritating substances, including bacteria, thus the risk of infection increases. Skin that is macerated is more prone to friction, which means that tissue can tear more easily.
How is Wound Moisture Controlled?
You might wonder how wound moisture can be perfectly controlled to enhance, rather than delay, wound healing. These days, there are numerous dressings available that are designed to wick moisture away from the wound bed when wounds show signs of being too moist; there are also dressings that can donate moisture to an overly dry wound bed, while others maintain the status, quo, so to speak.
Besides dressing, there are other wound management strategies that help to control wound moisture. For example, controlling bacteria is also important. Infected wounds are often too moist. Wounds that require debridement are usually too dry, and removing necrotic tissue will reveal a moist wound bed that will heal much more rapidly.
As can be seen, maintaining a moist (but not too moist!) wound environment is important in wound management and healing. If you enjoyed this article and would like to learn more about wound care certification, visit Wound Educators, specializing in preparing you to become a certified wound professional.
Source:
Meyers, B. (2008). Wound Management: Principles and Practice. 2nd edition. Pearson Prentice Hall. Upper Saddle River, New Jersey. pg. 124-125.
Liu, G. (2011). Optimizing the Wound Healing Environment. Nursing Excellence, the online newsletter for children’s nurses. http://www.childrenscentralcal.org/PressRoom/Publications/NursingExcellence9/Pages/OptimizingWoundHealingEnvironment.aspx

Hi. I like all your articles. Thank you very much. Do you have any article about responsibilities for wound care nurse? Thank you.
Here are some articles about wound care nursing
WOUND CARE SPECIALTY FOR NURSES https://woundeducators.com/wound-care-specialty/
WOUND CARE SPECIALIST https://woundeducators.com/wound-care-specialist/
From Sri Lanka
I did my fibroid operations in 1999
After I had a.big pain in my left leg and
Doctors never identified
Later after 3 months came to know I Had a Dvt
Still having more pains with ulcer
Let me know how to cure it
I recommend you be seen by a certified wound specialist. To find a specialist in your area visit: https://portal.abwmcertified.org/ABWMweb/Directory/ABWMcontent/Directory.aspx
Great article. Thanks for sharing it.
Very informative & helpful! Thank you so much!
Have a moist wound on the scalp behind the left ear for almost a year. Don’t recall how I got it. It will not heal using a liquid bandage.
My theory it won’t heal is that when lying down involuntary head movements while sleeping rub off
the liquid bandage. The pillow covering gets moist and gets me awake. Keeping the wound covered with a large bandaid is more comfortable by keeping the moisture out. Each time the bandage was changed the old bandage was wet. Got tired of this and went to the liquid bandage. It’s good But a regular large bandaid controlled the moisture.
Can’t leave my home due to imbalance preventing doctor office visits. An example of how things work is
the Oak Street medical clinic is four blocks from my home won’t send a doctor. However, Aetna
Medicare sends me a doctor from Philadelphia 60 miles away. Both Oak Street and Aetna Medicare
are owned and operated by CVS Pharmacy.
Refer to comment awaiting moderation explaining home confinement due to imbalance preventing doctor office visits for a behind left ear excessive water wound. It appears doctors are too lazy to make home
visits. The local Reading Hospital does not have doctors making home visits. My wife and I as well as
our friends and neighbors figure it’s more money for them to have you hospitalized than making home
visits by a doctor.
hello, thank you for your insightful and well-educative resources. Please can you help me with the diagrammatic illustration of the moist wound healing theory by George D Winter, 1962. or any conceptual framework done on the theory? Thank you