Phases of Wound Healing- Part 1
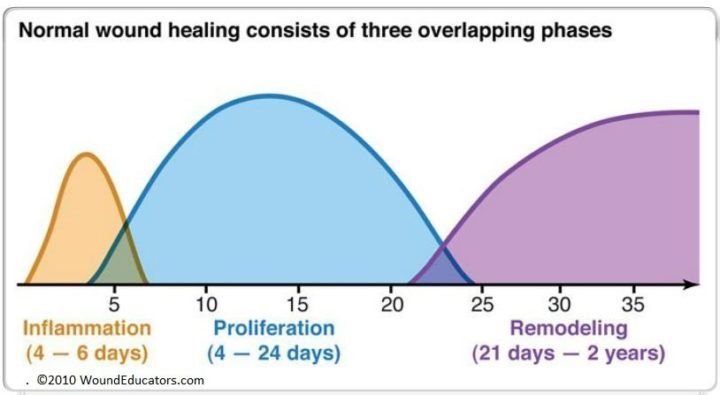
Wound healing proceeds in a relatively organized fashion, following three processes that overlap- inflammation, proliferation and maturation/remodeling (some sources will describe this process as four phases breaking the inflammation process into hemostasis and inflammation). How much do you remember about the phases of wound healing? First, let’s take a look at the inflammatory phase, which occurs right after injury.
Inflammatory Phase
We sometimes tend to think of inflammation as undesirable, but in reality inflammation serves many important functions, such as controlling bleeding and preventing infection. The inflammation phase begins immediately following injury and lasts for several days. In addition to controlling bleeding and preventing infection, inflammation also sets the stage for healing because it signals cells that are responsible for repair and regeneration to come to the site of injury.
Vascular response
- blood vessels contract and a clot is formed- the injured blood vessels allow fluid to leak out of the blood vessels into the surrounding tissue, causing localized swelling; this fluid is called transudate, made up of salt, water and proteins
- platelets travel to the site of injury and aggregate both together and to the injured endothelium; activated platelets release chemical mediators
- once bleeding is controlled and hemostasis is achieved, blood vessels dilate again to allow essential cells to reach the wound site; activated platelets release chemical mediators including cytokines (signaling proteins), growth factors (hormone-like substances that control cell growth and differentiation) and chemotactic agents (which attract the cells necessary for wound repair)
- as the blood vessels dilate, more fluid is forced into the interstitial space, which permits more inflammatory cells and growth factors to reach the area of injury; the mixture of protein, fluid and white blood cells is called exudate, which is thicker and more viscous than transudate and is creamy to yellowish in color
- histamines released by mast cells cause short term vasodilation; prostaglandins released by injured cells cause more prolonged vasodilation- this vasodilation results in the characteristic signs and symptoms of inflammation: redness, warmth, swelling, pain and decreased function
Cellular response
In addition to the vascular response described above, there is an equally important cellular response that occurs during the inflammatory phase:
- increased vasodilation causes a decrease in local blood volume, which results in a slowing of circulating white blood cells known as polymorphonuclear neutrophils (PMNs), which are then pushed to the outer margins of the blood vessel walls (margination)
- PMNs migrate through capillary walls (known as diapedesis), forcing their way through the interstitial space by extending pseudopods (small, foot-like projections) through narrow openings within the blood vessel walls; PMNs migrate toward the site of injury toward the highest concentration of the chemical gradient formed by changes in pH, bacterial toxins and dead/dying cells (a process known as chemotaxis)
- PMNs are the first scavengers to reach the injury site, usually within 12 to 24 hours; PMNs secrete inflammatory mediators and chemotactic agents such as interleukin-1, which attract even more PMNs capable of phagocytizing bacteria
- monocytes are next on the scene; monocytes are capable of killing pathogens and direct the repair process, also producing growth factors. Monocytes mature into macrophages once they leave the circulation
As you can see, inflammation is necessary and desirable. We often try to dampen the inflammatory process, but it is not necessarily a bad thing unless it is prolonged or very excessive.
Wound healing is a complex, and rather amazing, sequence of events. Phases of wound healing do not occur in a linear fashion but proceed in an overlapping fashion. If you find wound education interesting, perhaps you should consider pursuing online wound care education. Wound Educators can help prepare you for wound care certification. Contact us today!
Sources:
Myers, B. (2008). Wound management: Principles and practice. Pearson Education Inc., Upper Saddle River, New Jersey pp 12-16.
Mercandetti, M & Cohen, A. Wound healing and repair. Medscape. Updated April 2013. http://emedicine.medscape.com/article/1298129-overview#a1
Armstrong, D & Meyr, A. Wound healing and risk factors for non-healing. Up to Date. Updated November 2012. http://www.uptodate.com/contents/wound-healing-and-risk-factors-for-non-healing
What is the difference between a PMN and a macrophage?
Although both are phagocytes, they also have some specialized functions. The PMN is the first phagocyte recruited to sites of inflammation. They are loaded with lytic enzymes, and are very efficient at phagocytic killing. Macrophages are less capable of phagocytic killing unless activated, but they can also serve as antigen-presenting cells, thus they can help in the activation of helper T cells.

Hi Laurie,
Dr. Weiss here. I work at the Morrison Center in NYC. I’m writing a blog on prolotherapy and platelet rich plasma for our patients. I really like the wound healing graphic – it’s simple and elegant. Will you grant permission for us to use the graphic for our blog?
Thanks!
Dr. Weiss
Hi Dr. Weiss, You are free to use our graphic, however, I kindly request that you add woundeducators.com to the image. Best Regards, Laurie
An interesting discussion is worth comment.
I do think that you should publish more about this
issue, it might noot be a taboo matter butt typically people do not
discuss such issues. To the next! All the best!!